The end-to-end automation layer for modern 340B programs
Plenful’s 340B Audit & Optimization Suite fully automates a 100% audit of eligible 340B claims, uncovers missed savings and intelligently streamlines the referral capture process.






















Covered Entities face intense pressure to manage regulatory complexity and protect 340B savings
Compliance Exposure & Program Vulnerability
Manual audit processes make it nearly impossible for 340B programs to scale. Teams are often limited to spot audits—leaving thousands of claims unchecked and exposing programs to compliance risk. Misclassified claims, inconsistent data, and messy audit trails only compound the problem. Without a centralized platform to track, search, and validate claims activity, teams remain anxious about audit readiness and the potential for findings that could jeopardize their program eligibility.
Missed Savings from Fragmented Workflows
Siloed data and rigid eligibility logic create blind spots that hide millions in potential 340B savings. Referral data is often scattered across disparate systems, making it a “needle in a haystack” to find eligible claims. The result: missed opportunities, inefficiencies, and a lack of clear visibility into program performance. Most Covered Entities don’t have the bandwidth or analytics infrastructure to uncover these insights—let alone act on them.
Changing Legislation & Program Requirements
New and evolving policies—like the 340B Rebate Model Pilot and Medicare Drug Price Negotiation Program—are reshaping the 340B landscape. These changes will require teams to rapidly adapt operational processes, reporting structures, and financial oversight models. The organizations that succeed will be those that modernize early—using automation to stay compliant, nimble, and financially resilient amid growing regulatory complexity.
Streamline your compliance efforts. Maximize savings recapture. Sleep at night.
Built for 340B teams, Plenful’s 340B Audit & Optimization suite centralizes your disparate claims data, automates claim-level logic, and delivers actionable insights—turning hours of manual review into minutes of intelligent validation.
Strengthen Compliance Posture
Validate 100% of eligible 340B claims against HRSA requirements and your Covered Entity’s Policies & Procedures through automated verification. Plenful works across owned, contract, and mixed-use settings.
Recapture Missed 340B Savings
Pinpoint high-value claims that should qualify for 340B pricing but were incorrectly classified as ineligible, recapturing lost revenue quickly and confidently.
Referral Capture & Network Transparency
Automate referral pathway verification with provider matching and documentation tracking across your network to uncover additional savings recovery from referral-based prescriptions.
Plenful automates over 95% of the work for messy, disparate administrative workflows
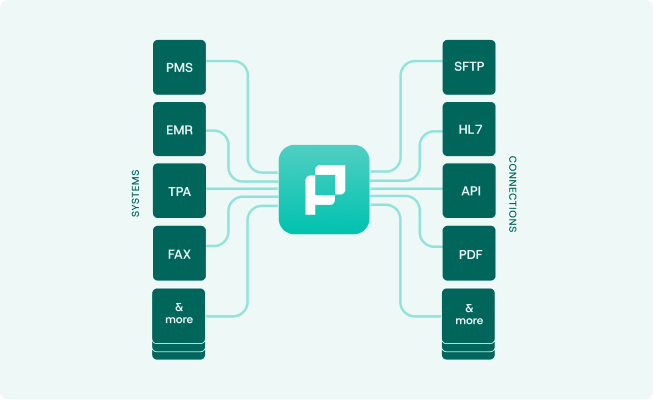
Connect Your Disparate Data Systems
Plenful connects to EHRs, TPAs, and fax systems to centralize fragmented 340B data. Standardized data creates the foundation needed to power audit, missed savings, and referral capture workflows at enterprise scale.
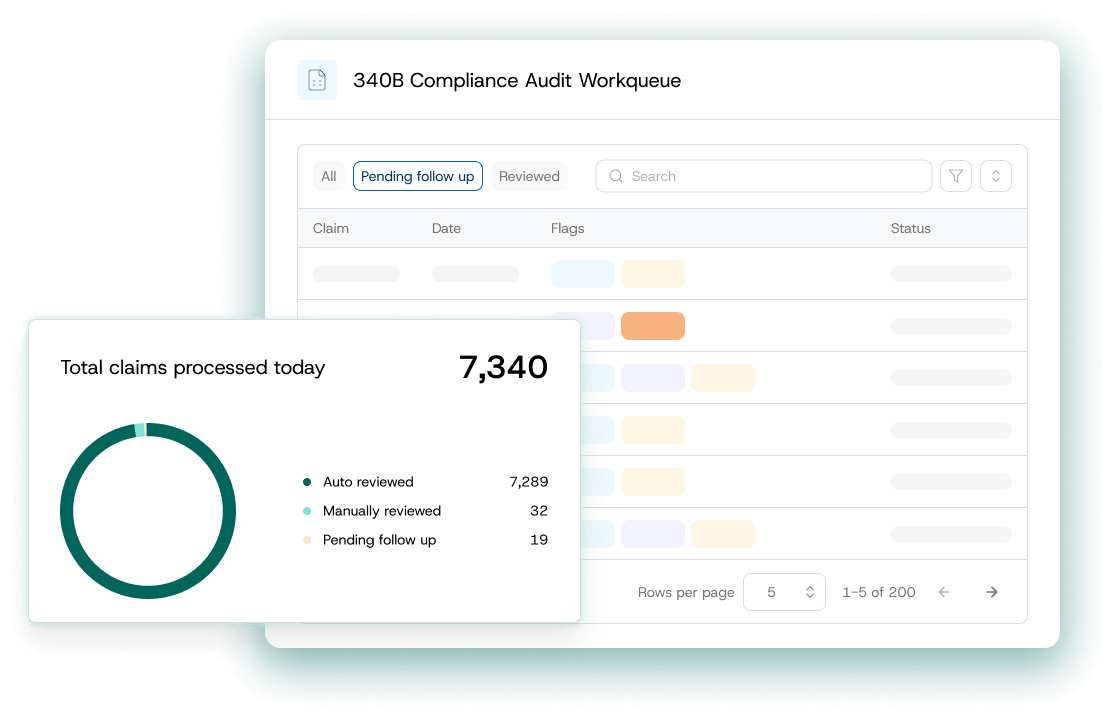
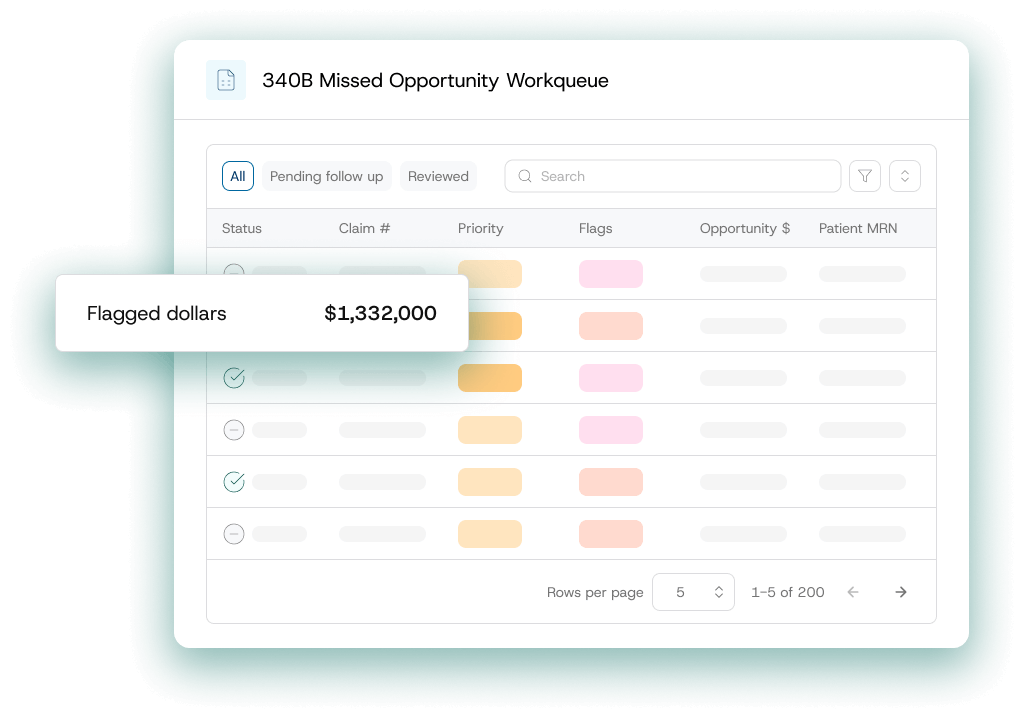
Analyst Task Management & Workflow Prioritization
Empower 340B analysts with an easy-to-use task management portal that surfaces the highest-value claims for review and action. Plenful’s configurable workspace allows users to set custom filters, flags, and queues aligned with their existing workflows. Track tasks from identification through resolution, maintaining full visibility and accountability while saving hours of triage.
AI-powered Referral Capture
Plenful leverages large language models (LLMs) to automatically review unstructured EHR data—scanning clinician notes for referral indicators and surfacing eligible opportunities that would otherwise require manual review. Integrated through FHIR, the platform connects documentation across systems, flags potential referral prescriptions, and prioritizes high-value claims for review.

Executive 360 Dashboards & Insights
Plenful brings fragmented claims data into a single, summarized view. Track KPIs, monitor program performance, and demonistrate measurable ROI from one executive dashboard.

Trusted by 90+ Enterprise Healthcare Organizations
"Utilizing Plenful helps me sleep at night, knowing our 340B program is compliant. With Plenful, we're now auditing 100% of our 340B claims."
Thomas Kim