Increase infusion capacity by 4x, accelerate time to therapy
Plenful automates intake and prior authorization workflows from end-to-end, helping infusion teams reduce delays, improve coordination, and expand capacity without increasing headcount.





















Infusion operations are stuck in the 90s, creating serious capacity bottlenecks
Rising Demand, Outdated Systems
Infusion therapy demand is growing 7–11% year over year, but operational systems haven’t kept pace. Teams are forced to manage higher volumes with the same manual, disconnected workflows — leading to longer wait times, staff burnout, and revenue leakage.
Delayed Infusion Therapy Starts
Faxed referral packets require hours of manual review, sorting, and triage. These slow, paper-heavy processes delay therapy starts, strain staff capacity, and create friction across the entire patient onboarding workflow.
Lack of Real-Time Operational Visibility
Infusion leaders struggle to see where authorizations stand, how staff are performing, or where process gaps exist. Without data-driven insights, resource planning and performance optimization are guesswork.
Automation That Moves Infusion Care Forward
Plenful’s AI-powered platform automates every step of the infusion intake process — reducing administrative burden, improving time-to-therapy, and giving leaders the insights they need to scale operations sustainably.
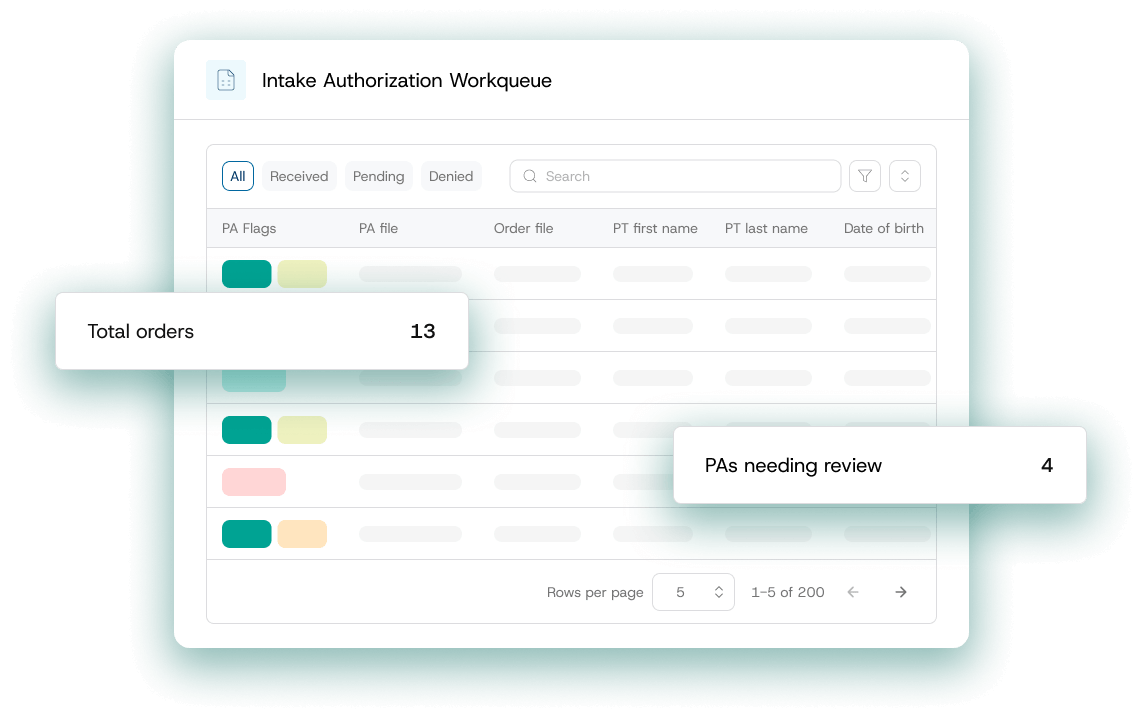
Unified Intake & Referral Processing
Plenful automates the referral process, extracts key data from any format and identifies missing data.
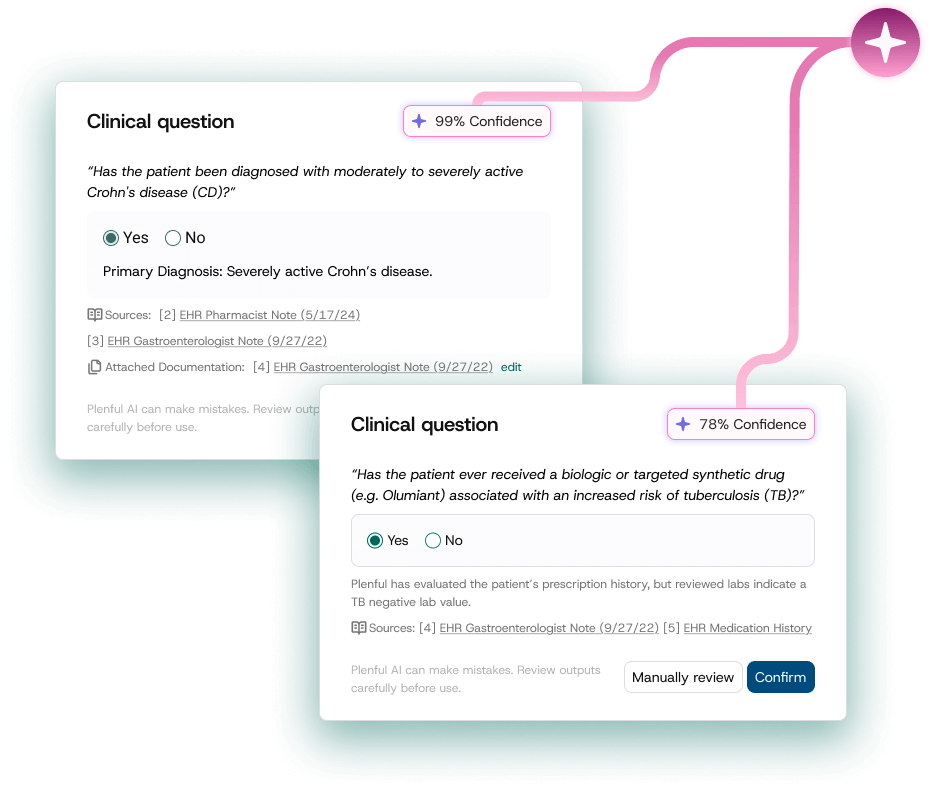
Intelligent Prior Authorization
Our LLMs reason and analyze across disparate patient documentation to pre-fill complex prior authorization requirements, eliminating redundant work and reducing manual work by up to 75%.
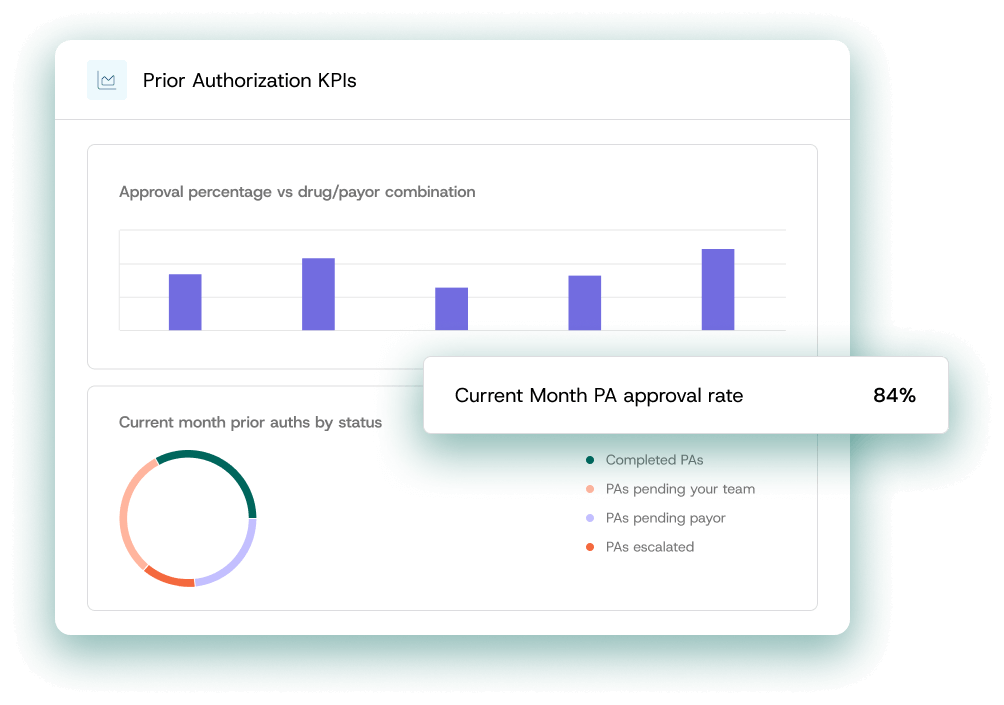
Operational Visibility & Optimization
Executive dashboards reveal where delays occur and where capacity can grow — helping infusion leaders optimize staffing and monitor finacial performance.
Plenful delivers a 4x capacity increase with end-to-end infusion workflow automation
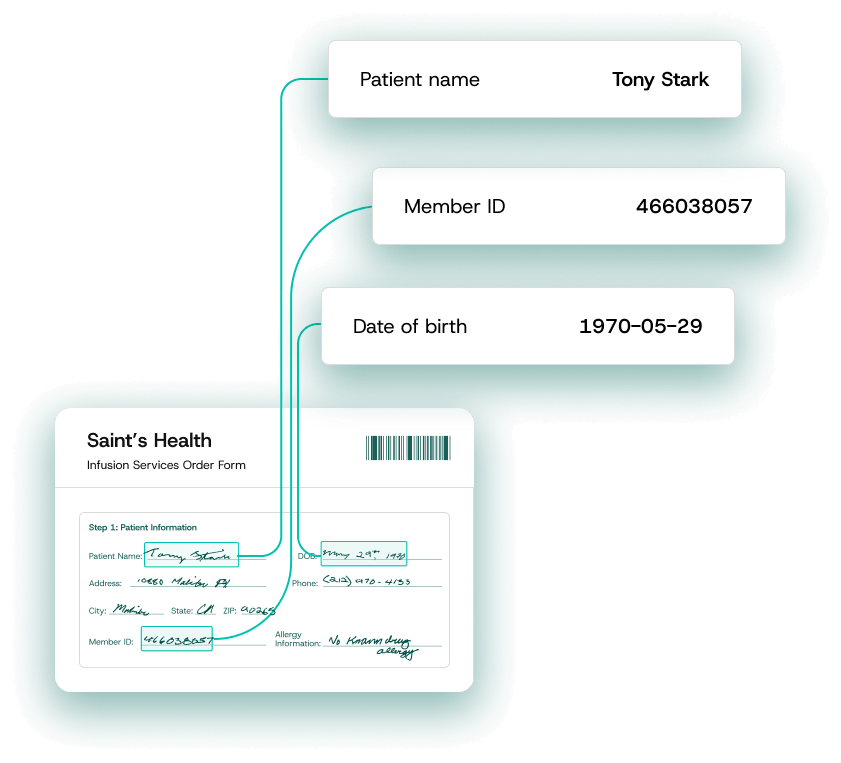
Intelligent Document Processing
Automatically read and normalize messy data from faxed referral packets to automate intake and processing. Plenful parses the data so it can be repositioned and integrated back into the EHR or Infusion Management System.
Streamline Infusion Prior Authorizations
Plenful’s LLMs automatically pre-fill complex prior authorization forms, using deep reasoning across patient medical history, payor rules, and clinical documentation. Submission TATs improve as the platform learns and fine-tunes from your team’s expertise and adjustments.
Executive 360 Dashboards
Track performance with dashboards that surface key metrics like throughput, turnaround time, and approval rates. Gain full visibility into financial and operational performance to protect margin and drive continuous improvement.

Trusted by 90+ Enterprise Healthcare Organizations
"Plenful’s solution has been critical for us. Since partnering with Plenful, our team's capacity has grown 4x, allowing us to focus on patient care instead of drowning in paperwork. Plenful isn’t just another tech vendor trying to 'disrupt' with shiny AI tech; they understand what we deal with every day and have built something that actually uplevels our operations."